Documenting Decline in Hospice: A Clinical and Regulatory Guide for Medicare-Certified Agencies
Understand the importance of documenting patient decline in hospice care. Learn how accurate records support Medicare eligibility, compliance, and quality care for certified hospice agencies.

Accurate and consistent documentation of patient decline is one of the most critical responsibilities in hospice care. For Medicare-certified hospice agencies, this documentation not only supports the clinical picture but also defends the patient’s continued eligibility for services under the Medicare Hospice Benefit. Surveyors, auditors, and Medicare Administrative Contractors (MACs) rely heavily on how decline is captured in the clinical record—making high-quality documentation essential for compliance, billing, and ethical care delivery.
This article outlines what hospice agencies must document to show patient decline and how to do so effectively across clinical visits, recertification periods, and interdisciplinary group (IDG) meetings.
Why Documentation of Decline Is So Important
The Medicare Conditions of Participation (42 CFR Part 418) require hospices to demonstrate that a patient’s prognosis remains six months or less if the terminal illness runs its normal course. At each benefit period—especially the third benefit period and beyond—hospices must show ongoing clinical decline.
Poor or vague documentation is a leading cause of claim denials, especially during targeted probe and educate (TPE) reviews or post-payment audits. MACs and surveyors expect to see evidence of decline that is measurable, observable, and directly tied to the terminal illness and related conditions.
Key Areas to Document Decline
Hospice staff should consistently evaluate and chart decline across multiple domains. Here's what to capture:
1. Functional Status and Activities of Daily Living (ADLs)
Describe changes in mobility, toileting, bathing, eating, and dressing.
Use objective tools like the Palliative Performance Scale (PPS) or FAST scale (for dementia).
Example: “Patient now requires maximum assistance with all ADLs; previously ambulated 10 feet with walker, now bedbound.”
2. Nutritional Intake and Weight
Record exact intake patterns and recent weight changes.
Avoid vague terms like "poor appetite"—instead, quantify food and fluid intake.
Example: “Patient consumed less than 25% of meals this week; weight decreased from 110 lbs to 105 lbs.”
3. Cognitive and Neurological Status
Document orientation, alertness, communication ability, responsiveness, and safety awareness.
Example: “Patient increasingly somnolent, awakens only to painful stimuli; disoriented to person and place.”
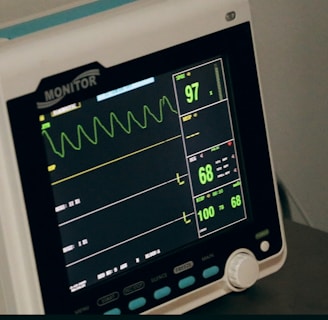
4. Vital Signs and Physiological Indicators
Track blood pressure, heart rate, respiratory rate, oxygen saturation, and temperature.
Show instability or progressive decline in baseline values.
Example: “BP 88/50, RR 28 with increased work of breathing, O2 sat 89% on 3L.”
5. Pain and Symptom Burden
Use validated pain and symptom assessment tools (e.g., numeric scale, PAINAD).
Document frequency and effectiveness of interventions.
Example: “Patient reports pain 8/10 in abdomen despite scheduled morphine; PRN dose provides temporary relief.”
6. Skin Integrity and Infection
Note presence of pressure ulcers, skin breakdown, or recurrent infections.
These signs often indicate terminal decline and increasing care needs.
Example: “Stage 3 pressure ulcer to sacrum with foul odor and purulent drainage.”
7. Psychosocial and Emotional Indicators
Describe withdrawal, anxiety, spiritual distress, or end-of-life planning conversations.
Example: “Patient stated ‘I’m ready to go’ and began discussing funeral arrangements with family.”
Best Practices for Documentation
To ensure defensibility and accuracy, follow these proven documentation tips:
Be Specific and Objective
Avoid general statements. Use numbers, timeframes, and comparisons to previous function or assessments.
Instead of: “Patient appears weaker.”
Use: “Patient unable to sit upright unassisted today; previously able to sit up for 15 minutes.”
Track Decline Over Time
Use progress notes to show a trend in deterioration, not just a single snapshot. This helps establish eligibility through recertification periods.
Individualize the Narrative
Use free-text areas in the EHR to add detail that drop-downs can’t capture. Include patient or caregiver quotes when relevant.
Example: “Daughter reports patient no longer responds to voice and refuses all food for past 3 days.”
Link Clinical Findings to Prognosis
Explain how observed decline supports the expected life expectancy of six months or less.
Example: “Decline in oral intake, bedbound status, and increasing somnolence consistent with terminal trajectory.”
Recertification Documentation
During recertification (especially after the 180th day), documentation must clearly justify the patient’s continued eligibility. This includes:
Recent PPS or FAST score comparisons
Clinical progression of terminal illness
Worsening of comorbidities
IDG notes reflecting agreement with continued eligibility
If decline is not obvious, documentation should show why hospice is still appropriate—e.g., unstable symptoms, recurring infections, or inability to function independently.
Avoiding Common Documentation Pitfalls
🚫 Using vague phrases: “Patient stable,” “No complaints,” or “Continues on hospice.”
✅ Instead: Describe what “stable” looks like (e.g., “Pain continues at 6/10 with nightly exacerbation.”)
🚫 Failing to explain PRN use or symptom management.
✅ Document frequency of use and symptom response to medications.
🚫 Omitting psychosocial or caregiver burden observations.
✅ Include caregiver reports, spiritual concerns, and bereavement indicators.
Final Thoughts
For a Medicare-certified hospice, documenting decline isn’t just about checking a box—it’s about painting a full, defensible picture of the patient’s journey. Your notes must clearly show how the patient’s condition aligns with hospice eligibility and how care is being delivered in response to ongoing decline.
With precise, narrative-rich documentation, your agency not only remains in compliance—it upholds the mission of hospice: providing compassionate, end-of-life care rooted in dignity, quality, and understanding.


